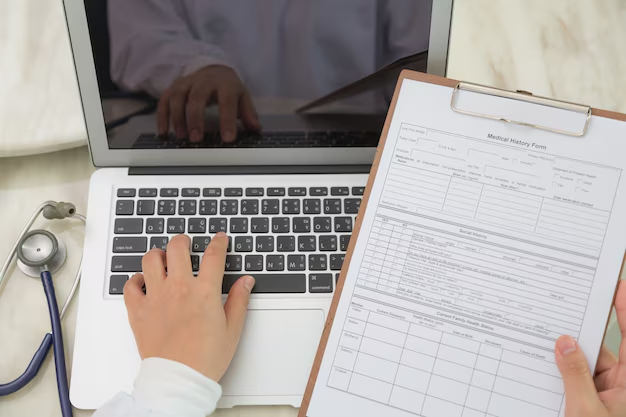
Medical Billing and Coding
We handle the entire medical billing and coding process, from accurate claim submission to seamless payment posting, ensuring faster reimbursements and fewer denials. Our team of certified coders uses the latest ICD-10, CPT, and HCPCS coding standards to guarantee precision and compliance with healthcare regulations.

Claims Submission and Follow-Up
We handle the entire claims submission process with precision, ensuring that every claim is coded accurately and submitted on time. Our proactive follow-up team tracks claims in real time, quickly addressing denials and resubmitting claims to minimize revenue loss.

Revenue Generation Cycle
We manage the entire Revenue Cycle from patient registration to final payment posting, ensuring a seamless and efficient billing process. Our expert team optimizes every stage, including insurance verification, claims submission, follow-ups, and denial management, to maximize reimbursements and reduce payment delays.

Payment Posting
We ensure accurate and timely payment posting to keep your revenue cycle running smoothly. Our team meticulously records and reconciles payments from insurance providers and patients, minimizing discrepancies and preventing revenue loss

Denial Management
We take a proactive approach to denial management, ensuring that every denied claim is reviewed, corrected, and resubmitted promptly. Our expert team identifies root causes of denials, whether due to coding errors, missing information, or payer policy changes, and implements strategies to reduce future rejections.

Patient Billing and support
We provide a transparent and hassle-free patient billing experience, ensuring that patients receive clear, accurate, and timely bills. Our team manages statement generation, payment processing, and account inquiries, making it easy for patients to understand their financial responsibilities.
With dedicated support specialists, we assist patients with billing questions, payment plans, and insurance coverage explanations. By offering friendly and professional assistance, we help improve patient satisfaction while ensuring timely collections and reduced outstanding balances.
Credentialing & Provider Enrollment
We help providers get enrolled with insurance networks and maintain credentials, ensuring compliance and preventing reimbursement issues.

Customized Reporting & Performance Analysis
Get detailed insights into your practice’s financial performance with our custom reports and analytics, helping you track trends and make informed decisions.

Prior Authorization & Eligibility Verification
Before treatment begins, we verify patient eligibility and obtain prior authorizations from insurance providers, reducing claim denials and ensuring timely approvals.

Our Commitment to Excellence
At PrimeLink, we believe that medical billing should be accurate, efficient, and stress-free. Our core values define who we are and guide us in delivering the best services to healthcare providers. We are committed to integrity, innovation, and client satisfaction, ensuring seamless medical billing solutions that maximize reimbursements and minimize errors.
Accuracy
Every claim we process is handled with the utmost attention to detail, reducing errors and ensuring timely reimbursements.
Integrity
We believe in honest and ethical medical billing, keeping our processes clear and ensuring no hidden costs.
Security
Patient data is sensitive, and we strictly adhere to HIPAA and other healthcare regulations to ensure confidentiality and security.
Efficiency
We prioritize quick and smooth billing operations to help healthcare providers receive payments without unnecessary delays.
Innovation
We leverage the latest medical billing technologies and automation tools to enhance accuracy and productivity.
